We are pleased to offer Integrated Behavioral Health services that allow patients to receive care for behavioral/mental health conditions through their primary care provider at a Morris Hospital Healthcare Center. Integrated Behavioral Health is a care delivery approach that treats the “whole person” by equipping the primary care provider (family medicine, internal medicine, pediatrician) with additional teammates and resources in order to address the patient’s physical health AND behavioral/mental health concerns in the primary care setting.
At Morris Hospital & Healthcare Centers, one of our guiding principles is that mental health IS health. Our approach encourages patients to bring all of their concerns about their physical health and mental health to their primary care provider, including:
- Depression/Grief
- Anxiety
- Bipolar Disorder
- Post-Traumatic Stress Disorder
- Addictions/Substance Use Disorders
HOW DOES INTEGRATED BEHAVIORAL HEALTH WORK?
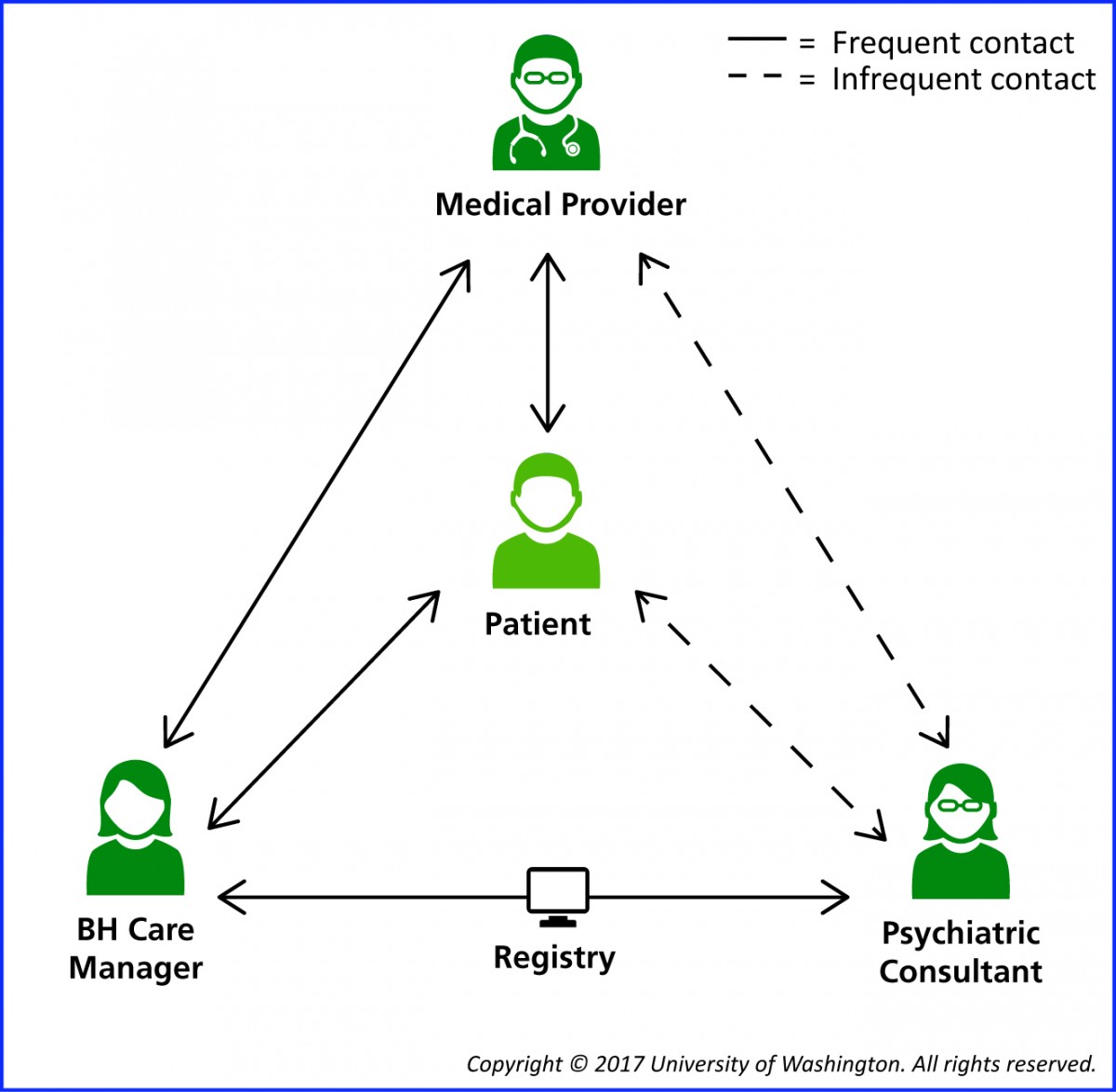 There are many models and approaches to Integrated Behavioral Health. At Morris Hospital, we use a Collaborative Care Model (CoCM), which is team-based care delivered in the primary care/medical office setting. In addition to your primary care provider, the Collaborative Care Model includes a behavioral care coordinator and a psychiatric consultant. The behavioral care coordinator provides brief counseling and case management from the primary care office setting, checking in with patients between visits with the primary care provider. The psychiatric consultant provides support to the team and makes treatment recommendations, including medications that may be prescribed by the primary care provider.
There are many models and approaches to Integrated Behavioral Health. At Morris Hospital, we use a Collaborative Care Model (CoCM), which is team-based care delivered in the primary care/medical office setting. In addition to your primary care provider, the Collaborative Care Model includes a behavioral care coordinator and a psychiatric consultant. The behavioral care coordinator provides brief counseling and case management from the primary care office setting, checking in with patients between visits with the primary care provider. The psychiatric consultant provides support to the team and makes treatment recommendations, including medications that may be prescribed by the primary care provider.
WHAT ARE THE BENEFITS OF RECEIVING BEHAVIORAL HEALTH CARE IN THE PRIMARY CARE SETTING?
For as long as modern medicine has been in practice, primary care has been vital in addressing health issues. Often viewed as the patient’s most trusted medical professional, a primary care provider guides patients through a wide variety of health care needs while building lasting relationships with their patients, delivering compassionate care, striving to prevent potential health issues, and pointing their patients to reliable specialists when more advanced care is required.
Our Integrated Behavioral Health services care for the whole person – both mind and body – in the primary care provider setting so that treatment for depression and anxiety can come as easily for a patient as treatment for a cough or earache.
HOW DO I GET STARTED?
The first step involves making an appointment with a primary care provider at a Morris Hospital Healthcare Center to discuss your behavioral health concerns. Together, you will decide if collaborative care is the right fit for your behavioral health needs. If not, your primary care provider will help connect you to the appropriate level of behavioral health care.
To find a primary care provider at a Morris Hospital Healthcare Center, please follow this link to the Primary Care page on our website.
FREQUENTLY ASKED QUESTIONS:
Where can I find a primary care provider with Morris Hospital’s Integrated Behavioral Health Services?
More than 20 primary care providers and obstetrician/gynecologists offer Morris Hospital’s Integrated Behavioral Health services. If you are experiencing behavioral health concerns and already have an established patient relationship with one of our primary care providers or OB/GYNs, please schedule an appointment with them to discuss your concerns. If you aren’t currently established with a Morris Hospital primary care provider, please go to the Primary Care page on our website to select a location and provider.
Can I receive treatment for substance use or addiction concerns?
It is our goal to partner with you, the patient, to develop a plan that meets your needs. If you need additional care for substance use concerns, many of our providers have additional training and experience in the field of addiction medicine. Our team can also help connect patients to a higher level of care for substance use disorders if needed.
What is the patient’s role in the treatment process?
The patient is the most important person on the team and receives the best care by participating actively with their primary care provider and behavioral care coordinator. Patients should let their primary care provider and behavioral care coordinator know what’s working for them and what’s not working, help track their progress, ask questions about their care, and take medications as prescribed.
Can I choose my behavioral care coordinator?
Your primary care provider will connect you with the behavioral care coordinator that’s part of the primary care provider’s team. If you feel your behavioral care coordinator isn’t the right fit for you, you should talk with your primary care provider.
Will I meet the psychiatric consultant?
The psychiatric consultant works to support and advise the care team on a shared plan of care. Within the Collaborative Care Model, the psychiatric consultant does not see you for a direct evaluation, but rather, works in conjunction with your primary care provider and behavioral health care coordinator to development a treatment plan with you at the center. This team based approach allows the psychiatric consultant to help many more patients.
Can I have appointments with my behavioral care coordinator through telemedicine?
While in person visits in the office are always encouraged, you can schedule video or phone appointments with your behavioral care coordinator if needed. Many patients do a combination of in-person and telemedicine visits.
How long will I receive Integrated Behavioral Health services?
Most patients receive behavioral health treatment through our collaborative care model for 3-6 months. At the end of the episode of care, you will continue seeing your primary care provider for periodic check-ups. If your behavioral health condition worsens, you can start seeing your behavioral care coordinator again for a new episode of care. If your needs exceed what we can offer through the collaborative care model, your team will help connect you to a higher level of behavioral health services.
How are behavioral health services billed through the collaborative care model?
You will be billed through your primary care provider’s office for visits with the primary care provider and for time spent with the behavioral care coordinator, including in-person, video and telephone visits.
MEET OUR BEHAVIORAL CARE COORDINATORS:
Dawn Harris, LCSW
 Dawn Harris is a Licensed Clinical Social Worker who serves as the Behavioral Care Coordinator for the Minooka Healthcare Center – Mondamin Street and Morris Hospital Ottawa Campus.
Dawn Harris is a Licensed Clinical Social Worker who serves as the Behavioral Care Coordinator for the Minooka Healthcare Center – Mondamin Street and Morris Hospital Ottawa Campus.
Dawn has been employed at Morris Hospital as a Behavioral Care Coordinator since July 2020. She earned her master’s degree from Loyola University Chicago and her bachelor’s degree from Northeastern Illinois University in Chicago. She has been counseling adults for more than 16 years.
Dawn believes in the collaborative care model as it provides patients an opportunity to receive care for mental health symptoms in a primary care setting, therefore, breaking down barriers to treatment and providing patients an opportunity to improve their lives by treating all aspects of their health.
Sheryl Janz, LCPC
 Sheryl Janz is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for the Minooka Healthcare Center at the Morris Hospital Ridge Road Campus.
Sheryl Janz is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for the Minooka Healthcare Center at the Morris Hospital Ridge Road Campus.
Sheryl has been employed at Morris Hospital as a Behavioral Care Coordinator since May 2019. She has a master’s degree and bachelor’s degree from Lewis University in Romeoville and has been counseling adults and adolescents for more than 20 years.
Sheryl is passionate about Collaborative Care Counseling and finds the comprehensive, short-term model to be very effective in providing integrated care and improving clinical outcomes for patients.
Katrina Neubauer, LCPC
 Katrina Neubauer is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for Morris Hospital Obstetrics & Gynecology Specialists.
Katrina Neubauer is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for Morris Hospital Obstetrics & Gynecology Specialists.
Katrina started with Morris Hospital in 2023. She completed her bachelor’s degree in psychology at Saint Xavier University and her master’s degree in clinical counseling psychology from Lewis University in Romeoville. Katrina has over 10 years of experience working with adults, adolescents, and children treating numerous mental health struggles in a variety of settings.
Katrina is passionate about the Collaborative Care Model as it unites physical and mental health concerns and integrates providers to deliver consistent care, along with improving the overall health of patients.
Ashley Norkus, LCPC
 Ashley Norkus is a Licensed Clinical Professional Counselor who serves as the behavioral health care coordinator for the Morris Healthcare Center-Dresden Drive.
Ashley Norkus is a Licensed Clinical Professional Counselor who serves as the behavioral health care coordinator for the Morris Healthcare Center-Dresden Drive.
Ashley started with Morris Hospital in 2023. She completed her bachelor’s degree at Aurora University and her Master’s degree in counseling psychology from Lewis University in Romeoville. Ashley has over 10 years of experience with adults and adolescents, treating various mental health and substance abuse issues in a variety of settings.
Ashley is passionate about the collaborative care model. She believes it is important to have early intervention to minimize symptoms and have integrated care with providers to treat all aspects of health and improve quality of life.
Carrie Skubic, LCPC
 Carrie Skubic is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for the Dwight, Diamond-Coal City and Morris (Lakewood Drive) Healthcare Centers.
Carrie Skubic is a Licensed Clinical Professional Counselor who serves as the Behavioral Care Coordinator for the Dwight, Diamond-Coal City and Morris (Lakewood Drive) Healthcare Centers.
Carrie has been employed at Morris Hospital as a Behavioral Care Coordinator since April 2024. She earned her master’s degree from Governor’s State University and her bachelor’s degree from Eastern Illinois University. She has been counseling a variety of ages for more than 20 years.
Carrie believes in the collaborative care model because it unites physical and mental health concerns and integrates providers to deliver consistent care. This collaboration can help improve the overall health and quality of life for patients.
Rebecca Tellez
 Rebecca Tellez is a mental health counselor who serves as the Pediatric Behavioral Care Coordinator under the Care Collaborative Model.
Rebecca Tellez is a mental health counselor who serves as the Pediatric Behavioral Care Coordinator under the Care Collaborative Model.
Rebecca has been employed by Morris Hospital since 2022 and serves as the first Pediatric Behavioral Care Coordinator to join the Care Collaborative Model. She has a master’s degree from Argosy University and bachelor’s degree from Loyola University.
Rebecca has 10+ years of experience with counseling and case management to a diverse group of patients across all demographics. Currently, she works with children and adolescents with a wide range of mental health concerns.
Rebecca believes greatly in the connection between mental and physical health, and finds this model of integrated care within pediatrics to be ideal for patients (and parents alike) to improve their overall health and well-being.
MEET OUR MEDICAL DIRECTOR:
Jennifer Thomas, M.D., FASAM
Dr. Jennifer Thomas , MD, FASAM, is a board-certified physician in family medicine and addiction medicine and currently serves as Medical Director of Integrated Behavioral Health at Morris Hospital. She completed her medical degree at SIU School of Medicine in Springfield, IL in 2007, and completed her family medicine residency at Hinsdale Hospital outside Chicago in 2010.
, MD, FASAM, is a board-certified physician in family medicine and addiction medicine and currently serves as Medical Director of Integrated Behavioral Health at Morris Hospital. She completed her medical degree at SIU School of Medicine in Springfield, IL in 2007, and completed her family medicine residency at Hinsdale Hospital outside Chicago in 2010.
Dr. Thomas completed the University of California Irvine Train New Trainers Primary Care Psychiatry Fellowship in 2018. As a leader in developing partnerships between academic research settings and community-based providers, Dr. Thomas works closely with the University of Washington AIMS Center. Dr. Thomas serves as Project Lead for Morris Hospital’s partnership with the AIMS Center’s NIMH-sponsored research study CHAMP: Collaborating to Heal Addiction and Mental Health in Primary Care. As an advocate for increasing access to medication for Opioid Use Disorder, particularly in rural settings, Dr. Thomas was part of an inaugural cohort of 5 IL physicians in 2021 supported by ISAM to become board certified in addiction medicine through the ABPM Practice Pathway.
Dr. Thomas is currently accepting patients with primary care psychiatry and/or addiction concerns. She sees patients at the Braidwood Healthcare Center of Morris Hospital and the Gardner Healthcare Center of Morris Hospital.
MEET THE PSYCHIATRIC CONSULTANTS:
Thomas Freeman, M.D., Child & Adolescent Psychiatry
 Dr. Thomas Freeman is a board-certified Child and Adolescent Psychiatrist and serves as a psychiatric consultant to the behavioral care coordinators and primary care providers through Morris Hospital’s Integrated Behavioral Health services.
Dr. Thomas Freeman is a board-certified Child and Adolescent Psychiatrist and serves as a psychiatric consultant to the behavioral care coordinators and primary care providers through Morris Hospital’s Integrated Behavioral Health services.
He completed his residency training at the University of Texas Medical School for General Psychiatry in 1989 and Washington University for Child and Adolescent Psychiatry in 2011. He received his Doctor of Medicine at the University of Texas Medical Branch in 1985.
He started his practice in general psychiatry and transitioned into child and adolescent psychiatry in 2011 after seeing a significant need in that population in underserved areas in rural Arkansas where he was practicing at the time.
Nelly Norrell, M.D., Psychiatry
 Dr. Nelly Norrell is a board-certified psychiatrist and serves as a psychiatric consultant to the behavioral care coordinators and primary care providers through Morris Hospital’s Integrated Behavioral Health services.
Dr. Nelly Norrell is a board-certified psychiatrist and serves as a psychiatric consultant to the behavioral care coordinators and primary care providers through Morris Hospital’s Integrated Behavioral Health services.
She completed her residency training at the University of Virginia, and previously received her Doctor of Medicine at the University of Arkansas for Medical Sciences in 2007. She specializes in geriatric psychiatry and completed her fellowship in 2021.
HELPFUL RESOURCES:
-
- NAMI Will/Grundy County: namiwillgrundy.org
- Behavioral Health Alliance of Grundy County: bhagrundycounty.com
- COLLABORATIVE CARE: aims.uw.edu/collaborative-care
- Mental Health America: mhanational.org
- National Institute of Mental Health: www.nimh.nih.gov


